Differences between bipolar- and depression
Contents
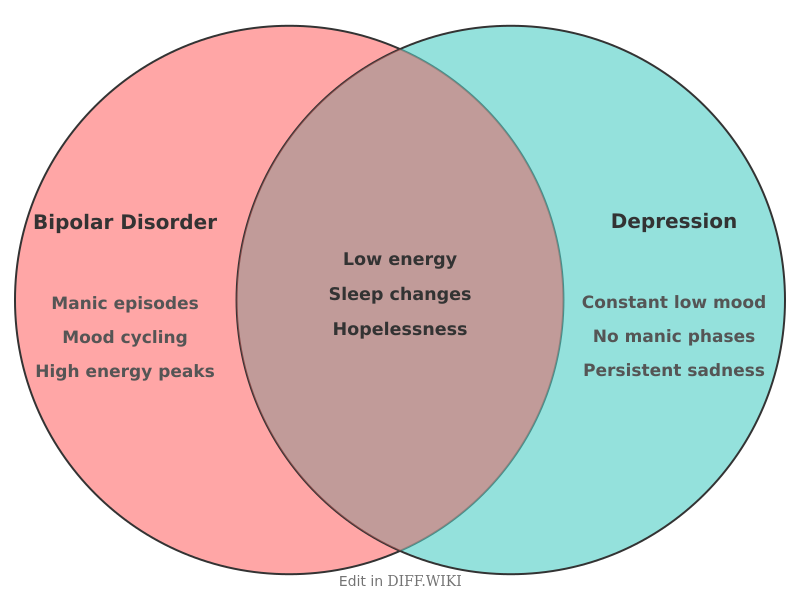
Bipolar disorder vs. Major depressive disorder
Major depressive disorder (MDD), often referred to as unipolar depression, and bipolar disorder (BD) are distinct clinical diagnoses categorized under mood disorders in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). While both conditions share the presence of depressive episodes, they differ in their clinical course, biological markers, and required treatments. The primary difference is the presence of mania or hypomania in bipolar disorder, which is absent in major depressive disorder.[1]
Comparison Table
| Category | Major Depressive Disorder | Bipolar Disorder |
|---|---|---|
| **Primary symptoms** | Persistent low mood, anhedonia, and fatigue. | Periods of depression alternating with mania or hypomania. |
| **Presence of mania** | Absent by definition. | Mandatory for diagnosis (Mania for Bipolar I, Hypomania for Bipolar II). |
| **Average age of onset** | Mid-to-late 20s. | Late teens to early 20s.[2] |
| **Genetic influence** | Moderate (approx. 35–40% heritability). | High (approx. 70–80% heritability). |
| **Sleep patterns** | Insomnia or hypersomnia during depression. | Decreased need for sleep during mania without feeling tired. |
| **First-line medication** | Antidepressants (e.g., SSRIs, SNRIs). | Mood stabilizers (e.g., Lithium) or anticonvulsants. |
| **Risk of antidepressant monotherapy** | Low; generally effective for symptom relief. | High; may trigger manic "switch" or rapid cycling. |
| **Psychosis** | Occurs only in severe depressive episodes. | Common during manic episodes and severe depressive states. |
Diagnostic differences
The diagnostic process relies heavily on a patient's longitudinal history. A patient currently experiencing a depressive episode may be misdiagnosed with major depressive disorder if their history of manic or hypomanic symptoms is not identified. Research indicates that the time between the first onset of symptoms and a correct diagnosis of bipolar disorder can exceed ten years.[3]
Manic episodes in Bipolar I disorder involve a distinct period of abnormally elevated or irritable mood lasting at least one week. Symptoms include pressured speech, racing thoughts, and inflated self-esteem. Hypomania, characteristic of Bipolar II, is a less severe form of elevation that does not require hospitalization or cause marked impairment in social functioning, though it must represent a clear change from the individual's baseline.
Treatment considerations
Pharmacological management differs significantly between the two conditions. In major depressive disorder, selective serotonin reuptake inhibitors (SSRIs) are frequently prescribed to increase synaptic serotonin levels. In bipolar disorder, however, using antidepressants without an accompanying mood stabilizer is associated with an increased risk of inducing a manic episode or increasing the frequency of mood swings.
Lithium remains a standard treatment for bipolar disorder due to its efficacy in reducing suicide risk and preventing future manic episodes. For major depressive disorder, psychotherapy—such as cognitive behavioral therapy (CBT)—is often used either alone or alongside medication. While psychotherapy is also utilized for bipolar disorder, it is generally considered an adjunct to medication rather than a primary treatment for the biological fluctuations of the disease.[4]
References
- ↑ American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.).
- ↑ Kessler RC, et al. (2005). "Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders." Arch Gen Psychiatry.
- ↑ Hirschfeld RM. (2003). "The Epidemiology and Burden of Bipolar Disorder." Journal of Clinical Psychiatry.
- ↑ Goodwin FK, Jamison KR. (2007). Manic-Depressive Illness: Bipolar Disorders and Recurrent Depression.