Differences between Acetaminophen and Ibuprofen
Contents
Acetaminophen vs. ibuprofen[edit]
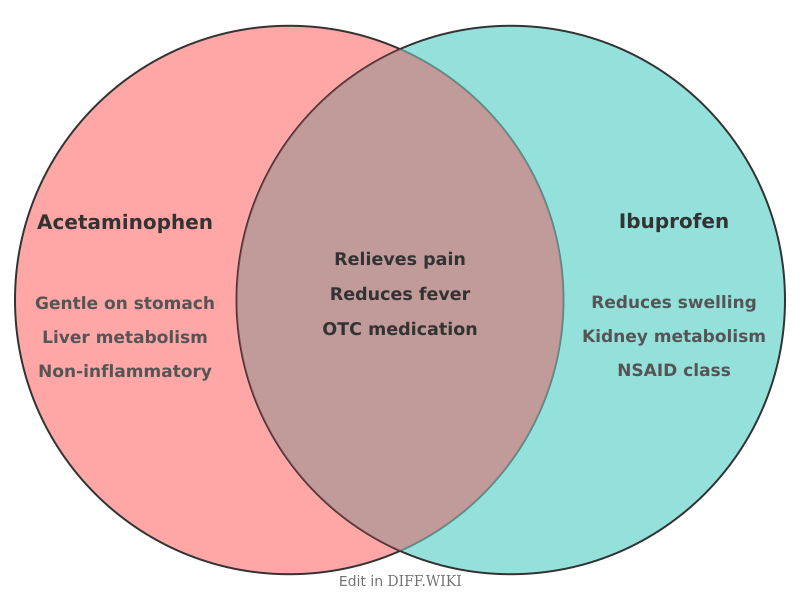
Acetaminophen (also known as paracetamol) and ibuprofen are two of the most common over-the-counter medications used to manage pain and fever. Although they are often used for similar symptoms, they belong to different pharmacological classes and have distinct safety profiles. Acetaminophen is classified as an analgesic and antipyretic, while ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID).
Comparison table[edit]
| Feature | Acetaminophen | Ibuprofen |
|---|---|---|
| Drug class | Analgesic / Antipyretic | Nonsteroidal anti-inflammatory drug (NSAID) |
| Anti-inflammatory action | Negligible | Significant |
| Mechanism of action | Central nervous system interaction | Inhibition of COX-1 and COX-2 enzymes |
| Common brand names | Tylenol, Panadol | Advil, Motrin |
| Primary organ of metabolism | Liver | Kidneys |
| Gastric impact | Gentle on stomach lining | May cause irritation or ulcers |
| Cardiovascular risk | Low | Potential increase in risk with long-term use |
| Standard adult dose | 500 mg to 1000 mg | 200 mg to 400 mg |
| Typical dosing interval | Every 4 to 6 hours | Every 6 to 8 hours |
Mechanisms of action[edit]
Ibuprofen works by blocking the production of prostaglandins, which are chemicals in the body that signal pain and cause inflammation. It inhibits the enzymes cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2). By reducing these enzymes in peripheral tissues, ibuprofen decreases swelling and redness at the site of an injury.[1]
Acetaminophen primarily acts on the central nervous system. While its exact mechanism is not fully understood, researchers suggest it increases the body's overall pain threshold. Unlike ibuprofen, it has very little effect on COX enzymes outside the brain, which means it does not reduce peripheral inflammation or swelling.[2]
Indications and efficacy[edit]
Both medications effectively reduce fever and relieve mild to moderate pain, such as headaches or toothaches. However, their specific properties make one more suitable than the other for certain conditions. Ibuprofen is generally preferred for inflammatory conditions, including rheumatoid arthritis, menstrual cramps, and muscle sprains, due to its ability to reduce swelling.
Acetaminophen is often recommended for patients who cannot take NSAIDs. This includes individuals with a history of stomach ulcers, blood clotting disorders, or kidney disease. It is also the preferred choice for fever and pain management in infants and children during certain viral infections, as NSAID use can sometimes be restricted based on specific medical histories.[3]
Safety and adverse effects[edit]
The safety of these drugs depends on the health of the organs responsible for processing them. Acetaminophen is processed by the liver. Excessive intake—either through a single large dose or chronic use—can lead to severe liver damage or failure. The maximum daily dose for a healthy adult is typically 3,000 mg to 4,000 mg. Alcohol consumption increases the risk of hepatotoxicity when taking acetaminophen.[4]
Ibuprofen is filtered through the kidneys and can affect the protective lining of the stomach. Frequent use may lead to gastrointestinal bleeding or decreased renal function. It is also associated with a slight increase in the risk of heart attack or stroke when used at high doses for long periods. Physicians often advise taking ibuprofen with food to mitigate stomach upset.[5]
References[edit]
- ↑ Mayo Clinic. (2023). "NSAIDs: Do they cause heart problems?"
- ↑ National Health Service. (2022). "Paracetamol for adults."
- ↑ Harvard Health Publishing. (2020). "Acetaminophen vs. ibuprofen: Which one for which pain?"
- ↑ U.S. Food and Drug Administration. (2022). "Acetaminophen Information."
- ↑ American Heart Association. (2021). "Nonsteroidal Anti-inflammatory Drugs and Cardiovascular Risk."